This blog, the third in an occasional series written by Digitunity’s Health Advisor, Amy Sheon, explores how healthcare systems can serve as effective channels for expanding digital access and opportunity. Read [Post #1] and [Post #2] to catch up on previous posts. The next installment will flip the perspective, focusing on how digital health tools can be embedded into community-based efforts to improve computer access and bridge the digital divide.
The World of Connected Health
Having a computer and internet are increasingly essential for maintaining health and managing illness. The benefits of technology for maintaining health, managing care and illness are summarized below.
Wellness
Being online enables people to find high-quality health information, find resources such as fitness classes and recreation areas, shop for healthy food, and find recipes to prepare. Connectivity also enables people to be in touch with family, find friends, and participate in activities that can boost well-being.
Apps on smartphones and wearable devices can help with tracking physiological state (sleep, menstrual cycles, mood, steps, and activity patterns). Many people find that the engaging nature of an “always on” device can provide greater self-awareness of behavior patterns and motivate change.
Managing Illness
Connectivity is especially helpful for finding appropriate care when needed for acute non-emergency situations such as a minor injury or sore throat. But it is especially valuable for addressing chronic illnesses such as diabetes and hypertension.
With the internet, people can remain in regular touch with their provider without going into an office. Patient portals are an invaluable one-stop shop for securely sending non-urgent messages to providers, ordering prescription refills, viewing lab test results and upcoming appointments, and, often, initiating a video visit.
Connected devices can also be used to track vitals such as blood pressure or weight. If monitored, providers can get an early indication of an exacerbation or problem that could be addressed before a crisis arises that might require an emergency room visit or hospitalization.
Considerations for Healthcare
We know that those who stand to benefit the most are least likely to be using digital health technology because of basic barriers that are often collectively referred to as “the Digital Divide.” As I and others describe elsewhere, individuals who are least ready for digital health have the poorest overall health.
When schools made the rapid transition to online education, they knew immediately that children from families that are poor, racial, and ethnic minorities, living in some rural and urban areas lacked connectivity. Digitunity has been instrumental in supporting heroic efforts in many communities to get laptops and hotspots to children.
The transition to online service in healthcare happened nearly as quickly as it did in education. However, healthcare faces some unique initial hurdles including needs for interoperability, protection of the privacy of patient data, and numerous regulatory changes to allow for the provision of care and payment for it.
Healthcare was several months behind education in recognizing that basic digital readiness gaps meant that older and sicker patients were either avoiding care altogether, continuing with riskier in-person care, or having audio-only telehealth visits. Such encounters lack the tremendous added value that comes with a two-way video encounter.
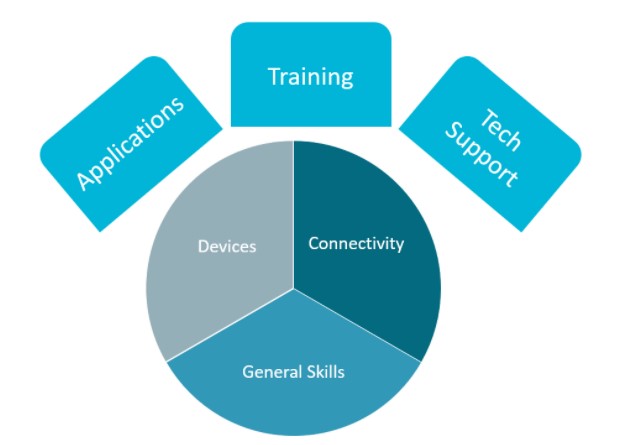
Digital Health Readiness
Common uses of technology generally require devices, connectivity, applications, and digital skills. Use of technology for healthcare may raise additional issues, either because of privacy and security considerations, or users may have health-related barriers.
These general & health-specific considerations are detailed below:
| Element | General Considerations | Health-Specific Considerations |
|---|---|---|
| Devices | ||
| Connectivity | ||
| Applications | ||
| Digital Literacy Skills |
Disseminating Digital Health Technology
A recent blog post detailed a series of strategies health systems can use to achieve more equitable adoption of digital health tools such as connected home monitoring devices, patient portals, and telehealth. This post reviews a range of specific strategies to prepare people for digital health. However, digital health readiness offers benefits that go far beyond healthcare, so some reframing is in order.
Treat Digital Health Readiness as a Social Determinant of Health (SDOH)

With longstanding interest devoted by the Robert Wood Johnson Foundation, the overwhelming effect of social determinants of health (SDOH), such as education, poverty, discrimination, segregation, inequitable access to healthy food, and recreation opportunities are now widely accepted by public health and healthcare leaders.
The U.S. vastly outspends other wealthy countries on healthcare, yet, sees far worse health outcomes. If a leaky roof isn’t fixed, a child who develops asthma from indoor mold will keep visiting the emergency room. If a senior cannot purchase healthy food because it costs more and they lack transportation to a grocery store, they will have difficulty managing diabetes or high blood pressure.
Both the public health and healthcare systems are now incorporating attention to SDOH. Each decade, the U.S. Centers for Disease Control and Prevention articulates population health objectives. Addressing SDOH is one of five overarching goals articulated in Healthy People 2030 objectives, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
Healthcare has also responded to SDOH. The Centers for Medicare & Medicaid Services (CMS) establishes policies that govern how healthcare for the majority of Americans is paid for. Private insurance often follows payment methods used in Medicare and Medicaid.
Since passage of the 2010 Affordable Care Act, payment for healthcare has shifted from “fee-for-service” to value-based models. Under the old model, providers were paid to see and treat patients, whether or not the treatment helped. In fact, if patients were harmed by care, like if they got an infection after surgery, the doctor would be paid even more to treat the infection.
Now, payment systems increasingly reward doctors and health systems for keeping patients healthy and reducing their use of emergency rooms and hospitals. In response to the shift in payment incentives, many health systems now screen patients for social needs that affect their health, and refer patients needing housing, utility, or food assistance to community organizations to address these needs.
Many use a common screening questionnaire to identify the needs and an electronic referral platform to connect the patient to the community organization. These “closed-loop” systems were developed to address the finding that up to 50% of social service referrals are not completed. Providers were often unaware of whether the patient obtained the needed services.
A Range of Options for Healthcare Sector Support for Digital Inclusion
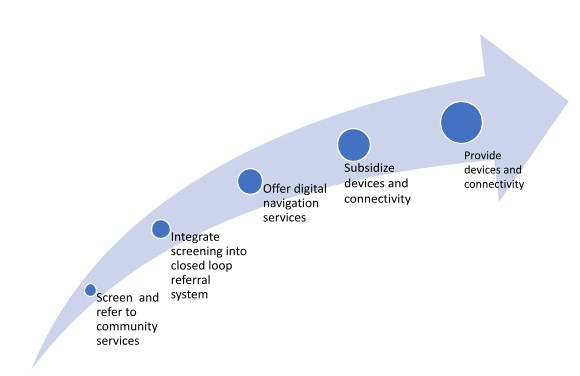
Many community health centers use a version of the Epic electronic medical record system that has a closed loop referral system built in, making it easy for the provider to make and track referrals. The jury remains out on whether these screening and referral programs will have the desired impact.
A common complaint is that the referral systems may require a separate login for the provider, a seemingly insurmountable barrier. One group of community health centers incorporated the closed loop referral directly in the electronic health record to avoid this extra step. Other health systems could encourage medical record software companies to integrate the closed loop referral system.
Offer Digital Navigation Services
The Affordable Connectivity Program included in the 2021 Infrastructure Investment and Jobs Act offers a $30 per month internet subsidy and $100 credit for household purchase of a connected device. However, finding a carrier with an available plan in their neighborhood and uploading documentation is daunting for a person who does not have the internet or strong digital skills.
Therefore, digital navigators, who are trained to understand patient needs and options, can be an invaluable bridge. The National Digital Inclusion Alliance is spearheading efforts to define and disseminate the digital navigator model. Meanwhile, DigitalUS offers a complete Digital Navigator Resource Hub and Playbook.
Subsidize Devices & Connectivity
In addition to screening and referring patients for digital readiness gaps, health plans could cover connectivity costs that exceed the ACP minimum and costs for those not qualifying for the ACP benefit. A single device costing under $100 is surely inadequate for a household with members simultaneously working from home, attending school online, and having a video call with a provider.
The door to Medicare coverage of internet services was opened by the 2020 program that allowed some private Medicare Advantage plans to pay for some “general supports” that have a “reasonable expectation of improving or maintaining the health or overall function of the chronically ill enrollee.” One recent review identified several Medicare Advantage plans that provide a cash benefit to cover expenses for internet and connected devices.
Understanding the possibility for Medicaid to cover costs of digital connectivity is more complex because the program is administered by states. Each state exercises considerable latitude in determining who is eligible for this insurance and what services are covered. CMS issued guidance in January 2021 to encourage state Medicaid plans to address SDOHs. However, the 52-page document does not mention devices, connectivity, or digital literacy training.
States can apply for waivers that might allow them to cover the cost of connecting patients, but pre-authorization has not been granted across the board. Which is disappointing, given the long list of services that have been pre-approved, including “housing-related services and support, non-medical transportation, home-delivered meals, educational services, employment, community integration, social support, and case management.”
I’m not a lawyer, but perhaps some of the approved services offer a window for covering digital devices and connectivity. For example, among families whose children are eligible for disability services, Medicaid reimbursement is available for “covered services included in the child’s IEP [individualized education plan] or IFSP [individualized family service plan] provided to eligible beneficiaries by qualified Medicaid providers.”
Perhaps these plans could specify the need for devices and connectivity as part of their plans. Similarly, “CMS supports states’ efforts to improve Medicaid enrollees’ health and well-being through incentivizing work.” Similar opportunities may be available through employment-related support. Ironically, the guidance notes that, “many services outlined throughout this document may be provided using telehealth modalities in addition to in person visits.
States are strongly encouraged to assess their telehealth frameworks to determine if there are unnecessary restrictions preventing maximum utilization of telehealth for the services appropriate to be delivered via telehealth.” Surely, lack of patient connectivity is a fixable issue that prevents maximum use of telehealth.
Direct Provision of Internet
Becoming an internet service provider is not a core competency of healthcare. However, a consortium of community health centers is testing provision of internet service to more than 3,400 low-income patients across Ohio, Oregon, and Washington. The program’s success will be known after completion of a three-year, $8 million Connected Care Pilot Program, funded by the Federal Communications Commission.
In Cleveland, local health systems are directly expanding broadband availability. The Cleveland Clinic is allowing DigitalC, a local non-profit broadband provider, to transmit wireless signal to the adjacent underserved neighborhood from its rooftop. MetroHealth System is funding DigitalC to provide low-cost broadband to nearby public housing units.
Providing Devices & Skill Training
No better evidence of the growth in attention to digital inclusion in healthcare is The Charles Benton Institute’s Digital Equity Champion Award being given for the first time in 2022 for work in the health sector. Ericka Camacho and John Torous, of Beth Israel Deaconess Medical Center were recognized for their exemplary work supporting digital inclusion for individuals with serious mental illness needing care during the COVID-19 pandemic.
Through the FCC’s COVID-19 Telehealth Program, $450 million has been designated to support health systems adopting telehealth, including making funds available to purchase devices for patients. This unprecedented program has been dwarfed by eye-popping resources included in the Infrastructure Investment and Jobs Act that cover provision of devices outlined below.
Infrastructure Act Programs That Can Support the Purchase of Connected Devices
- Broadband Equity Access & Deployment (BEAD) Program – $42 billion awarded to states for broadband deployment and adoption programs.
- Affordable Connectivity Program – $14 billion includes one-time discounts of up to $100 for qualifying households to purchase a connected device from a participating provider for a minimal fee.
- Digital Equity Act – $2.75 billion to ensure all individuals and communities can fully participate in the digital economy.
Learn More
This influx of funding for devices makes the Digitunity refurbishing model more important than ever. The subsidy will not cover high capacity devices, so refurbished devices will likely continue to play a vital role in closing device gaps. See the callout box below for how to donate or receive donated devices.
| Learn more about Digitunity's Device Donation Program: | Register your organization to receive technology donations: |
|---|---|
| https://social.digitunity.org/donate3 | https://links.digitunity.org/7LJO |
Technical Support
To ensure patients are able to use digital technology, health systems need to consider the types of training available for specific tools, such as telehealth or patient portals. Then, they must plan for problems that arise while using the technology. Training is a topic worthy of its own blog post, but in short, many technology companies offer training materials. Review them to make sure they meet the needs of patients with various types of digital vulnerabilities such as language, digital skills, and health literacy. If inadequate, consider making your own videos with input from patients.
The Tech Support team should anticipate the majority of calls to reflect basic digital skill gaps (e.g. recovering passwords or downloading apps), device capacity issues (e.g. microphone not working or no camera available), or connectivity problems (e.g. slow connections timing out or adjusting security settings).” While a health system may think of such matters as “not their problem,” resources must be in place to address them as they likely represent fundamental barriers to patient adoption of health technology.
One model to consider is training community health workers to serve as the first line of support, referring more difficult issues to individuals with more advanced technology support training. Training and certification of first-line tech support is available through Northstar, Literacy Minnesota, Grow with Google, or IBM edX. The resources listed above for Digital Navigators may also be of interest.
Measuring Success
Although data is seemingly at their fingertips, health systems generally do not track or report their success in connecting electronically with their patients, or helping their patients to get connected. Our local public hospital, MetroHealth, was the first to associate disparities in use of patient portals with disparities in neighborhood internet access.
Many have documented disparities in portal access and telehealth use. However, these metrics should be looked at in real time to monitor success in digital inclusion attempts. In my consulting practice, I advise leading health systems on how and what to track. The process could be scaled up if the electronic health record companies offered template reports on results.
In the meantime, kudos to Johns Hopkins Medicine for developing an algorithm to identify patients likely to need assistance before a telehealth visit. Such a model could easily be expanded to identify individuals likely to need assistance getting connected.
In other words, rather than screening patients one at a time, use the information known about their interactions with the healthcare system and the availability of affordable broadband in their neighborhood to proactively reach out to those least likely to be connected who might benefit most from connectivity.
Digitunity’s Opportunity Network Member Activity Related to Health & Healthcare
With the growing awareness across the healthcare sector in digital inclusion approaches, it’s no surprise that Digitunity’s Digital Opportunity Network members are offering creative solutions for reaching vulnerable patient populations. Digitunity works every day to direct donated computers to these organizations to benefit their clients. Meredith Wynne, Program Officer at Digitunity, shared a sampling of these organizations and their work below:
1. Digital Health Connectivity Project
The Digital Health Connectivity Project works across the United States to design tech-enabled solutions to the most pressing healthcare challenges facing vulnerable populations. Currently, they are collecting devices for families affected by the pandemic and enabling access for COVID patients in hospitals across the United States.
The Project also works closely with stakeholders across the health ecosystem to empower vulnerable populations to adopt telehealth solutions. Their HealthTech Literacy Project looks at the ways innovative health technologies create social inequalities in health and produces tailored communications, training guides, and resources to foster digital education development. You can learn more about their work here.
2. Findley Foundation, Inc.
The Findley Foundation assists individuals in becoming healthy, healed, and whole by providing vocational training, education, case management, healthcare, and behavioral health services in Wauwatosa, WI. They work to provide each senior below the federal poverty line with a computer to follow up with their physicians via telehealth tools.
During the roll out of the COVID-19 vaccine, the majority of seniors were unable to get vaccinated because they didn’t have the technology or ability to schedule an appointment. Findley provides a four week training to seniors and rewards them with a computer to schedule appointments via telehealth. You can learn more about the foundation’s training and other programs here.
3. Forever Captain Poodaman – The Ahmad Butler Foundation (ABF)
The purpose of ABF’s Coast to Coast Digital Learning Program is to give children battling cancer and other life threatening diseases the ability to continue to learn remotely while hospitalized. ABF donates computer charging carts and Chromebooks to children’s hospitals and children battling life threatening diseases in need. To learn more about ABF’s digital learning program, visit their website here.
4. Therapy Fund Foundation
The mission of the Therapy Fund is to facilitate access to quality mental health services, including telehealth, for Black people who suffer from racial trauma, anxiety, depression, and other ailments due to systemic oppression, economic sufferings, and intergenerational trauma that has not been addressed.
Qualified patients get vouchers for up to six therapy sessions to be used within a network of therapists selected for their cultural competence working with this population, including telehealth providers. The Therapy Fund also aims to support the tuition costs of Black clinicians who serve this community in Seattle, WA.
Digitunity recently began a partnership with the Therapy Fund. Donated computers will be used for staff and volunteers to help deliver their services, and youth participants to engage in telehealth therapy. You can learn more about the Therapy Fund and its services for clinicians and their clients here.
5. Alliance for Positive Change
The Alliance for Positive Change helps low-income New Yorkers living with HIV and other chronic health conditions to get the medical care, peer support, and housing assistance they need to achieve health, happiness, and stability.
They are working to expand access to telehealth treatment, care coordination services, opioid treatment, and behavioral healthcare. Their diverse range of individualized, professional services include access to healthcare, peer education, and safe-practice counseling.
The Alliance received 94 devices, keyboards, monitors, and mice through Digitunity’s efforts in 2020 for their clients to use to access telehealth services. Learn more about the Alliance’s programming, including telehealth, here.
Get Involved
If you’d like to learn more about Digitunity and their partners’ efforts to leverage healthcare for digital inclusion, you can contact Meredith Wynne here. If you’re looking to make a donation to one of the aforementioned organizations or any of Digitunity’s other partners, you can start the process on Digitunity’s donation matching platform here. Digitunity and their partner organizations thank you in advance for your support.
About the Author
Amy Sheon is a Digital Health Equity Consultant with, and President of Public Health Innovators, LLC. In addition to Digitunity, Amy advises leading health systems, educational institutions, non-profit, philanthropic, and government organizations on achieving and monitoring digital health equity.
She brings this message to industry through serving as a Board Member and Faculty for NODE.Health, the Network of Digital Evidence for Health. She is a member of the Data Collaborative Community of the Digital Medicine (DiMe) Society.


